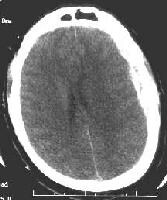
first define the term "subdural hematoma " as it is the most common of the two types of hematoma . Subdural hematomas are essentially a pooling or collection of blood between the dura (the brain's protective covering, or outer layer) and a part of the meningies known as the arachnoid. What this means is that blood is pooling and then settling on the brain's fragile tissue. Depending on the severity of the bleed and the pressure, this can be extremely serious and even life threatening. Typically, subdural hematomas are caused by head trauma of some kind like a car accident or violent movement like a shaken baby would experience. What most often happens is that a small group of veins near the brain, called bridging veins, tear or shear due to head trauma or violent shaking. Since these veins tear, they allow blood to seep out into the space between the dura and the meningies, causing what is called intercranial pressure (pressure on the brain).

Other causes of subdural hematomas are use of medications that thin the blood called anticoagulants; long term aspirin and ibuprofen use cause the blood to be thin and therefore make bleeds more likely. The elderly are often candidates for subdural hematomas due to weaker blood vessels and sometimes brain atrophy. Brain atrophy means that the brain becomes smaller which causes a pulling on the bridging veins, followed by tears (almost like a run in a pair of lady's stockings).
Other causes of subdural hematomas are use of medications that thin the blood called anticoagulants; long term aspirin and ibuprofen use cause the blood to be thin and therefore make bleeds more likely. The elderly are often candidates for subdural hematomas due to weaker blood vessels and sometimes brain atrophy. Brain atrophy means that the brain becomes smaller which causes a pulling on the bridging veins, followed by tears (almost like a run in a pair of lady's stockings).
The symptoms can include seizures, ataxia, lethargy, vomiting, visual problems, numbness, and ultimately coma and death. The best treatment for subdural hematomas are corticoid steroids to decrease swelling and surgery to alleviate pressure on the brain by draining some of the extra blood causing the pressure by drilling small holes in the cranium to release the access fluid.
In contrast, an "epidural hematoma" is caused by arterial tears as opposed to the tearing or shearing of veins. Also, the epidural hematoma is located outside of the dura, between the dura and the cranium. Epidural hematomas are often caused by head trauma, more specifically a blow to the side of the head that causes a fracture in the skull or temporal bone. Less than a third of epidural hematomas occur outside of the area of where the temporal bone is located. Epidural hematomas can be very dangerous and also life threatening, as about one in every five cases of people treated for the condition dies. Because epidural hematomas are essentially arterial bleeds, there is a greater volume of blood loss in a shorter period of time (arteries are larger than veins with larger blood volumes). As the intercranial cavity fills with blood, the dura can often strip away from the brain causing an extremely painful headache. This bleed from arteries can bring on symptoms much more quickly as the pressure increases more rapidly than with a subdural hematoma.
Epidural hematomas can also occur in the areas near the spinal cord as a rare complication from anesthesia or other surgeries. The treatment for epidural hematomas is a quick diagnosis (often during a lucid period experienced by the patient, a conscious state between states of unconsciousness which is a key characteristic of hematomas) followed by neurosurgery. Again, it is necessary to drill small holes into the cranium in order to relieve pressure on the fragile tissue of the brain. Without this surgery, death is eminent.
we hope that our sit usefull for you?
Sited:
www.nlm.nih.gov/medlineplus/enc/article000781.htm
en.wikipedia.org/wik/Epidural_hematoma
In contrast, an "epidural hematoma" is caused by arterial tears as opposed to the tearing or shearing of veins. Also, the epidural hematoma is located outside of the dura, between the dura and the cranium. Epidural hematomas are often caused by head trauma, more specifically a blow to the side of the head that causes a fracture in the skull or temporal bone. Less than a third of epidural hematomas occur outside of the area of where the temporal bone is located. Epidural hematomas can be very dangerous and also life threatening, as about one in every five cases of people treated for the condition dies. Because epidural hematomas are essentially arterial bleeds, there is a greater volume of blood loss in a shorter period of time (arteries are larger than veins with larger blood volumes). As the intercranial cavity fills with blood, the dura can often strip away from the brain causing an extremely painful headache. This bleed from arteries can bring on symptoms much more quickly as the pressure increases more rapidly than with a subdural hematoma.
Epidural hematomas can also occur in the areas near the spinal cord as a rare complication from anesthesia or other surgeries. The treatment for epidural hematomas is a quick diagnosis (often during a lucid period experienced by the patient, a conscious state between states of unconsciousness which is a key characteristic of hematomas) followed by neurosurgery. Again, it is necessary to drill small holes into the cranium in order to relieve pressure on the fragile tissue of the brain. Without this surgery, death is eminent.
we hope that our sit usefull for you?
Sited:
www.nlm.nih.gov/medlineplus/enc/article000781.htm
en.wikipedia.org/wik/Epidural_hematoma
JOIN OUR PAGE IN FACEBOOK



 7:09 AM
7:09 AM
 Unknown
Unknown